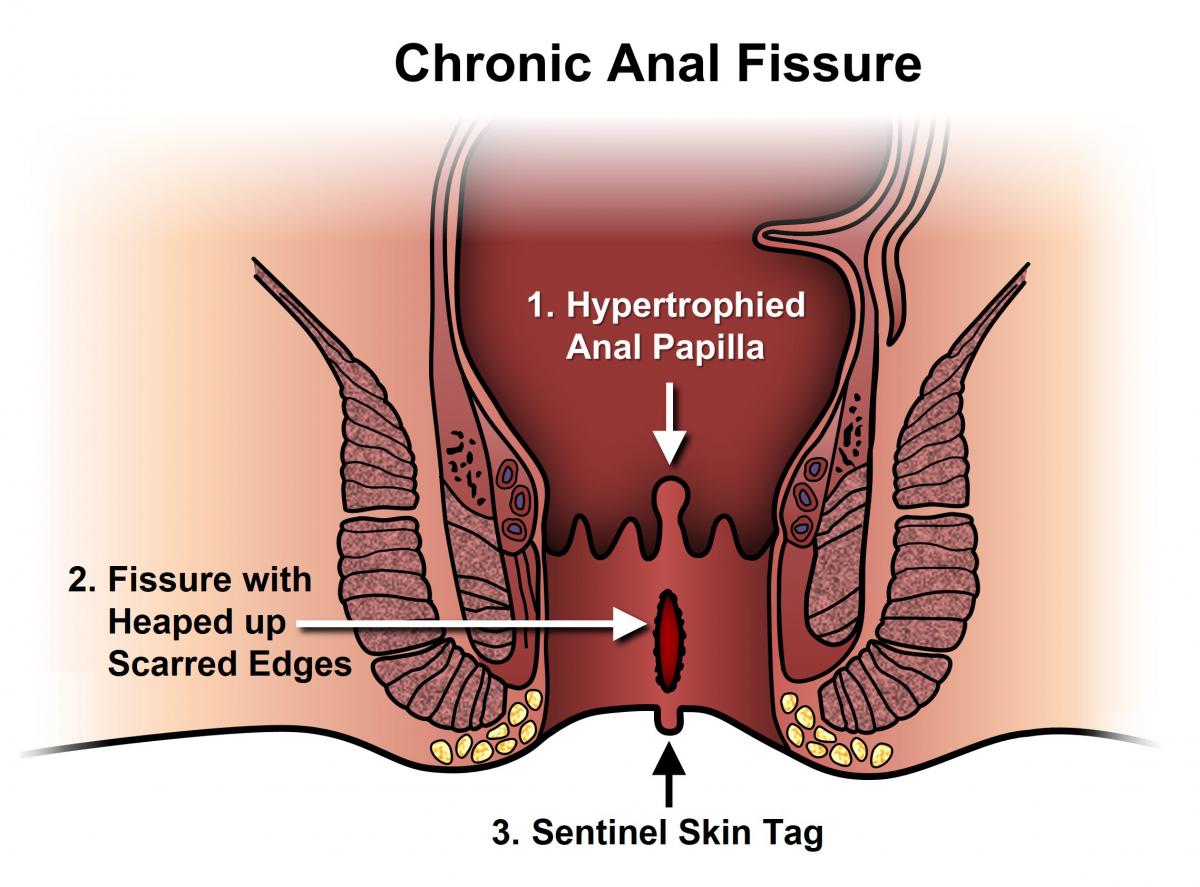
An anal fissure is a longitudinal tear or defect in the skin of the anal canal distal to the dentate line.
• Primary fissures are typically benign and are likely to be related to local trauma such as hard stools, prolonged diarrhoea, vaginal delivery, repetitive injury or penetration.
• Secondary fissures are found in patients with previous anal surgical procedures, inflammatory bowel disease (e.g. Crohn’s disease), granulomatous diseases (e.g. tuberculosis, sarcoidosis), infections (e.g. AIDS, syphilis) or malignancy
In approximately 90% of patients the anal fissure is located in the posterior midline. It is hypothesized that this predilection for the posterior midline may occur because this portion of the anal canal is poorly perfused. Anterior anal fissures affect approximately 10% of patients and may have a different pathophysiology. They are associated with younger, mostly female, patients often with an injury to or dysfunction of the external anal sphincter. In less than 1% of patients the fissures are lateral or multiple. Irrespective of these differences posterior and anterior anal fissures are thought to be of primary etiology, whereas lateral or multiple fissures are more likely to be secondary in nature.
The clinical features are severe tearing pain with the passage of feces often with a small amount of bright red blood on the stool or toilet paper.
A digital rectal examination is usually not needed to make the diagnosis and is contraindicated in many cases given the associated pain. However, examination under anesthesia with anoscopy, endoscopy, biopsy and imaging (i.e. CT scan, MRI or endoanal ultrasound) may all be required if:
• The fissure cannot be seen
• The diagnosis is unclear
• There is significant bright red bleeding in a patient with an increased risk for colorectal cancer
• There are features suggesting a secondary anal fissure
The differential diagnosis of a primary anal fissure is limited but includes a hemorrhoid, anal fistula or solitary rectal ulcer.
Conservative Management
The typical dosage of either 0.2% nitroglycerin ointment or 2% diltiazem cream is twice daily for 6–8 weeks. Other topical medications that you can find in a pharmacy commonly used in clinical practice are lignocaine and hydrocortisone. However, they have inferior healing rates to bran plus warm sitz baths.
The available evidence suggests that these injections of botulinum toxin probably have at least a similar efficacy (certainly not worse) to both topical glyceryl trinitrate and calcium channel blockers.
Surgical management
The timing of surgery is individual and variable: the literature often suggests 4 to 12 weeks. This procedure commonly involves division of the internal anal sphincter from its distal end to either the proximal end of the fissure or the dentate line (whichever comes first). Lateral internal sphincterotomy has an excellent healing rate of approximately 95%. Common complications include recurrence in up to 6% and incontinence of flatus or stool (usually transient) in up to 17% of patients.